There’s an old saying that tries to sum up the essence of Emergency Medicine: “know a little bit about everything rather than everything about a little bit”.
While the purpose of an emergency room may have started out well-intentioned, as a place to stabilize and treat the sickest patients any time of day, today’s version finds us in a very different role. We are the default solution: ‘let the ER handle it’. This means facing situations you may not have been trained on and being forced to work up patients for complications you might not be intimately familiar with. Take this hypothetical case I had a few weeks ago where the final diagnosis was one I had never heard of before…
Chief Complaint: “PEG tube broken”
An elderly woman presents to the ER complaining that she is unable to use her PEG tube today. At baseline, she cannot take anything by mouth and is completely reliant on the PEG tube for tube feedings to keep her nourished. The PEG was last changed about one year ago and she’s had no issues with it until today.
The ER nurse attempted to flush the tube with warm water with no success. Most of it ended up leaking out around the sides. This PEG tube needed to be changed. I grabbed an empty 10cc syringe and hooked it up to the port. I tried aspirating and nothing came – no air, no saline, nothing. It felt like I was trying to aspirate out of an empty balloon. I gently pulled on the tube and it wouldn’t budge. It seemed to be fixed to the abdominal wall. Puzzled, I ordered some basic labs, imaging, and started a liter of fluids. It was nearly midnight on a Friday night and I couldn’t just send this lady home with no plan for how to get through the weekend.
I called up the hospitalist, told a few jokes to grease the wheels, and managed to sneak in this patient for an admission and GI consultation in the morning. The following day, she was diagnosed with ‘Buried Bumper Syndrome’ and went to the operating room for removal/replacement.
BBS
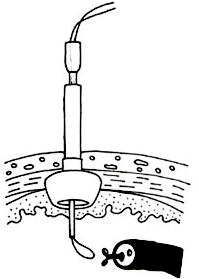
Buried bumper syndrome (BBS) is an uncommon and often late complication of PEG tube placement. It occurs when the internal bumper of the PEG tube erodes into the gastric wall and lodges itself between the gastric wall and skin.
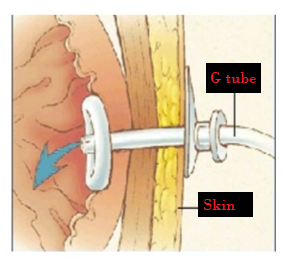
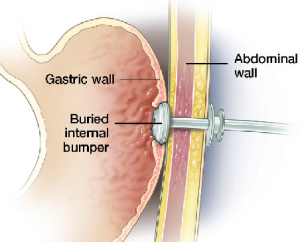
Normal PEG insertion Buried Bumper Syndrome
Patients typically have a triad of symptoms: a leaking tube, inability to infuse feedings or flush the tube, and a fixed, immovable tube. The mechanism for development of BBS involves excessive tension on the tube followed by ischemia and necrosis of the gastric mucosa by the internal bumper, with eventual migration into the abdominal wall.