Studies have shown that the average ER physician is interrupted once every six minutes. In a 12-hour shift, that comes out to over 100 times! Learning to work under such circumstances is just an expected part of the job. One of the most frequent interrupters is the triage tech who brings you ECG after ECG to sign off on. It can become easy to fall into a pattern of ‘STEMI or No STEMI’ and while that is the most emergent issue, there are some other things to note when handed an ECG (even if you aren’t going to ultimately be the provider caring for the patient). That patient may not be seen again for a few hours, so if there’s an arrhythmia or ischemia or peaked T wave, it can be important that the initial physician who signs off on the ECG catch it.
It’s also easy for the second provider to glance at the first provider’s interpretation (‘normal’, ‘no STEMI’, ‘WNL’, etc) and fall into a bias where they are basically expecting a normal ECG. But I cannot stress this enough: take a few extra seconds to really look at the ECG before dispositioning a patient. While this is true for everyone, I’m mostly looking at you: second provider who actually sees the patient.
This was the case of a middle aged man who presented with a fall. He had been seen a few months ago for the same thing. At that time, his heart rate was 50 and he was discharged home after a negative CT brain and no further workup. He returns after falling again for no apparent reason. There was an abrasion on the head but imaging was again normal. This time, the heart rate was 48, but labs were ordered and came back normal. Plans for discharge and close outpatient follow-up were made.
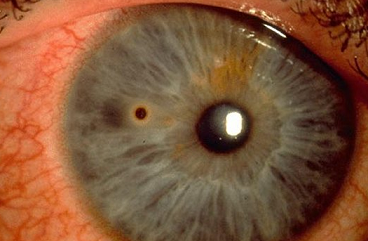
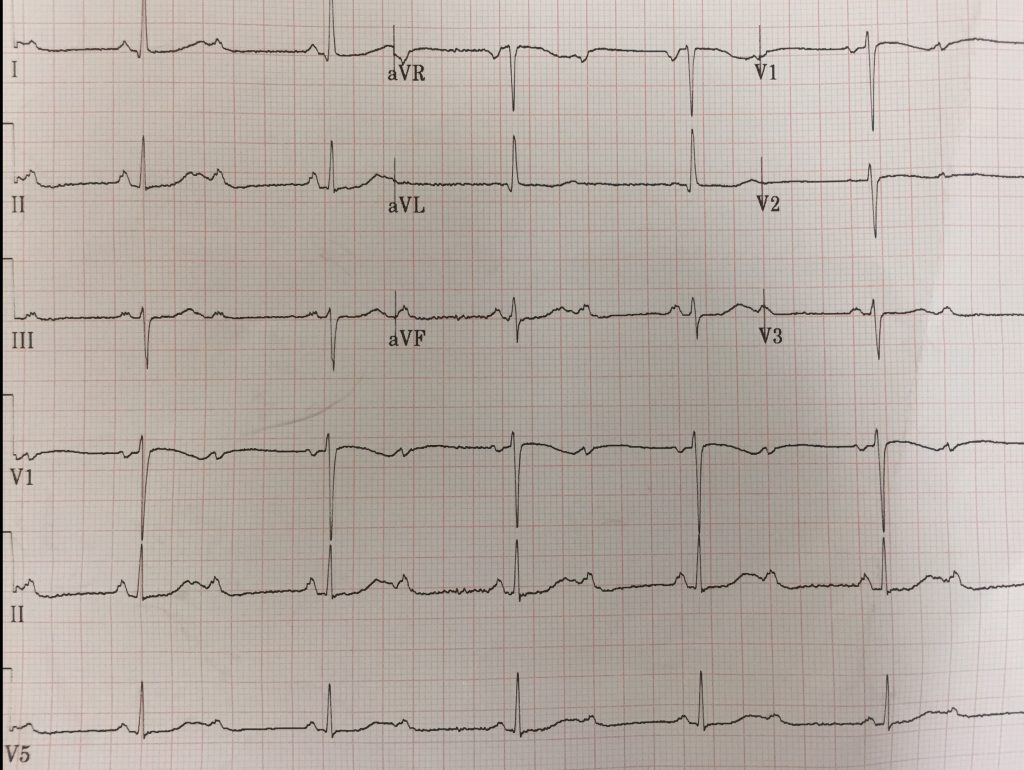
Just to be safe, I reviewed the first ECG again:
If you look closely, there’s something a little off about the T waves. They’re notched and broader than what one would expect.
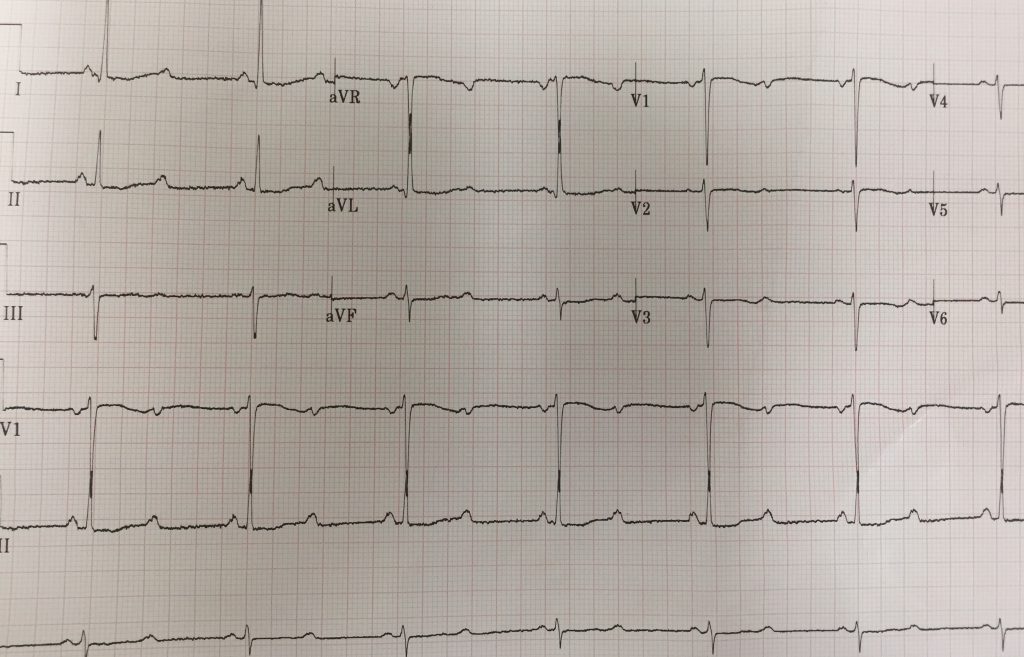
An ECG was repeated (it was now two hours later) and here is what was seen:
If you look at the rhythm strip, there are clearly p waves with dropped QRS complexes:
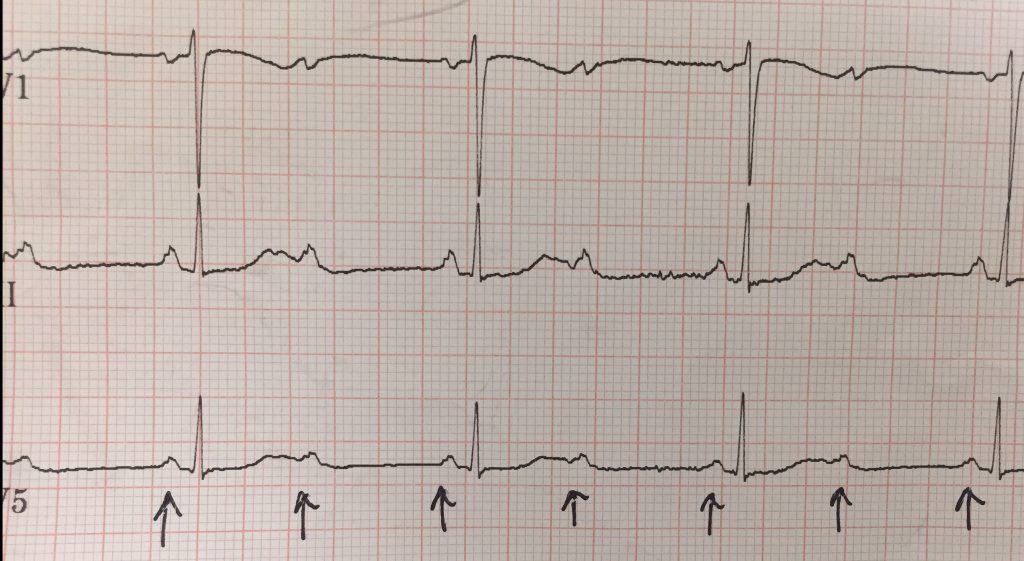
This patient has a second degree type 2 heart block (Mobitz II)!
A quick call to the cardiologist and the patient was admitted to the ICU to be safe. The following day she had a pacemaker inserted and went home.
Take-home points:
Don’t ignore abnormal vital signs. This patient was bradycardic for no reason (no medications and not exactly a well-built athlete).
When in doubt, repeat the ECG and cardiac enzymes.
Triple check ECGs! If you don’t look closely, you can miss something