Here’s the situation: it’s late, you’re hungry, and you can’t find a Taco Bell. Studies have shown that we don’t make good decisions when we’re hungry. Lunch breaks being a luxury for ED providers, we’ve all experienced that at some point. But I implore you – no matter how hungry you are or how far you have to drive, don’t make the same mistake as a healthy 25-year-old that came to the ED made: if you have to get fast food, drive the extra mile and go to Taco Bell.
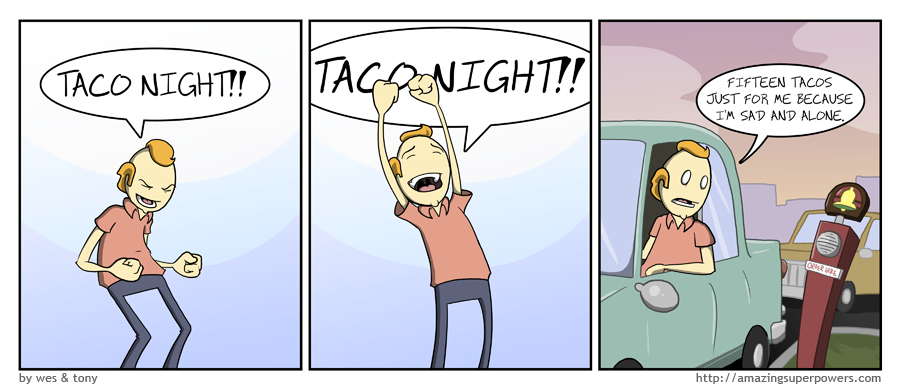
This person checked in for nausea and vomiting (no diarrhea) after making an ill-fated decision to go to Del Taco or some other generic rip-off of The Bell. He had no abdominal pain, normal vital signs, and was actively texting. The provider ordered PO Zofran and a PO challenge, with plan to discharge if things went according to plan. He remained nauseated so an IV was placed, Phenergan and fluids given, and labs sent off. Labs were normal. The patient felt better and was discharged home with ‘gastroenteritis’.
‘Gastro’ translates literally to ‘belly’ and ‘enteron’ is Latin for ‘intestine’
Inflammation of the lining of the colon typically manifests as diarrhea. Gastroenteritis can present without changes in bowel patterns, but it’s not very common.
The patient returned 12 hours later with persistent vomiting. Vital signs and labs again were normal, but this time he had left-sided abdominal pain. An acute abdominal series was ordered:
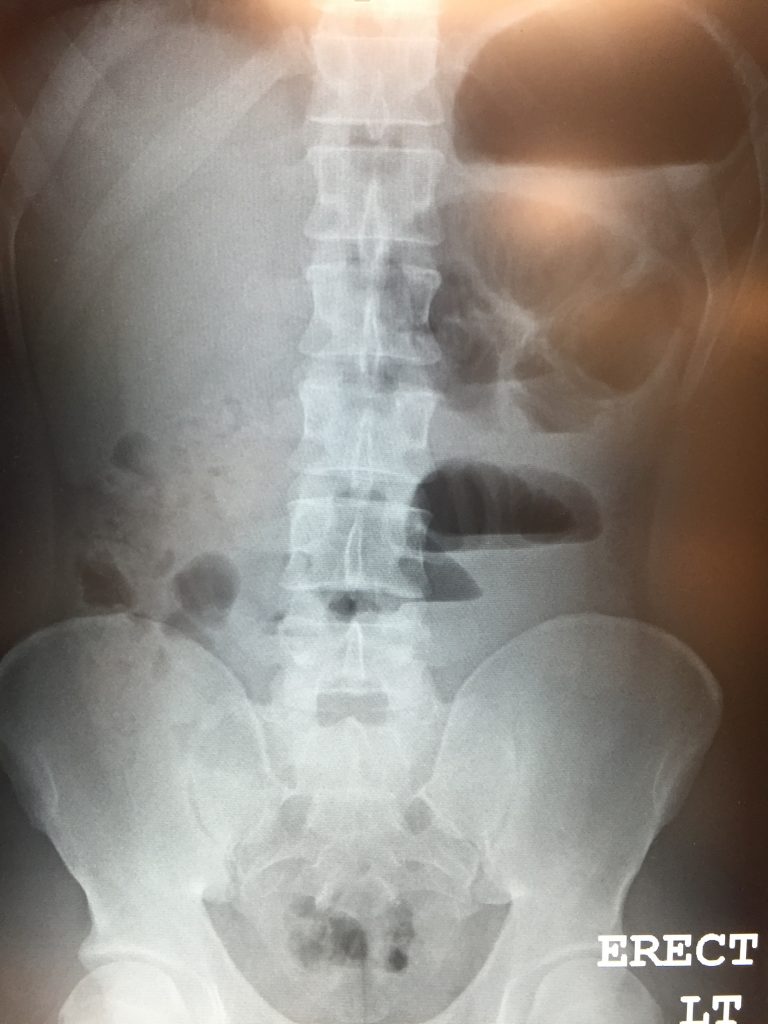
Interpretation:
Air-fluid levels in the small intestine
There is air present in the rectum so it’s not a complete bowel obstruction. The official interpretation is ‘ileus vs partial small bowel obstruction’.
Learning point:
Think twice about diagnosing someone with food poisoning or gastroenteritis in the absence of any intestinal symptoms. It’s certainly possible, but isolated vomiting should at least give you pause.




