It’s Okay to Be Wrong
A 50 year old female woke up at 2am with neck pain. She had a history of chronic neck pain but this was more painful than she had ever had before. EMS was called and her blood pressure was recorded as 170/90mmHg. In the ER, the nurse documented that the patient was visibly uncomfortable, complained of ‘pressure in her head’, and was diaphoretic.
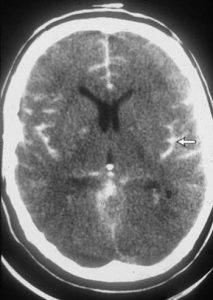
The ER physician documents a normal neurologic examination and lack of meningismus or neck stiffness. He specifically writes that the GCS is 15, ‘there are no carotid bruits, neck is supple, and there is no focal weakness’. In the medical decision-making section, the physician specifically documents that he considered CVA, meningitis, tumor, and intracranial hemorrhage but that based on history and exam, he has ruled out those things. The patient receives some pain medication, BP improves, and she is discharged home. A few days later she is brought back with severe headache and found to have a missed subarachnoid hemorrhage.
A lawsuit was filed against the original physician for failing to order an imaging study and failure to consider the most life-threatening causes. During his deposition, the prosecution focused on the role of an ER doctor in ruling out the most likely diagnoses to cause serious harm to a patient. His defense was that he did consider those diagnoses, and even documented it to show that he wasn’t being dismissive.
The case was eventually dismissed as they could not prove that the physician deviated from the accepted standard of care.
You can use clinical acumen to make decisions. Not everyone needs a CT scan or MRI. It makes things A LOT easier, but the standard of care is not to order tests on everyone to rule out the big bad stuff. The standard is to consider those diagnoses. Then use what the patient has given you to make a choice. It’s also better to document those diagnoses that you have considered, as well as how you ruled them out: rather than leaving them off the chart completely.
Clinical decision tools such as the Ottawa SAH criteria can help guide decision making regarding when patients may need further workup. This particular rule has shown 100% sensitivity for SAH, but can only be applied to very specific populations.
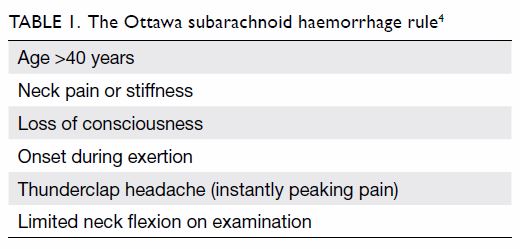
The Ottawa criteria can only be applied to patients over the age of 15 and they must have new, severe atraumatic headache with maximum onset within one hour.
Personally, I struggle to think of a situation where I would not image someone with new, severe atraumatic headache with maximum onset within one hour.