A 40-year old asthmatic presents to the ED with non-productive cough for two weeks. She has no other past medical history. She dropped her kids off at school, and being healthy and without a primary care physician, then drove herself to a hospital for some cough medicine and to sweet talk the doctors into some antibiotics.
To summarize: 40 years old. Healthy. 2 kids. And, worst of all for her, she was very nice.
It’s as anecdotal and contrived as “don’t say the ‘Q’ word”, but ask any EM physician and they’ll tell you that bad things happen to good people. Sure, gang-bangers get shot and hoodlums get stabbed over a few bucks. But it’s the bad news that you have to give to good people that you remember.
Despite normal vital signs and clear lungs, an x-ray was ordered. Maybe it was done because the provider had a tickling in their gut, maybe it was done because of the duration of the cough (two weeks), or maybe it was done because metrics demanded that we ‘stop the clock’ by ordering something (anything!) on a patient so someone who had never even seen the patient most likely read the chief complaint and ordered an x-ray:


Suspicious lesion in the right upper lobe and nodule in the left; seen again on the lateral view.
A CT chest was ordered:
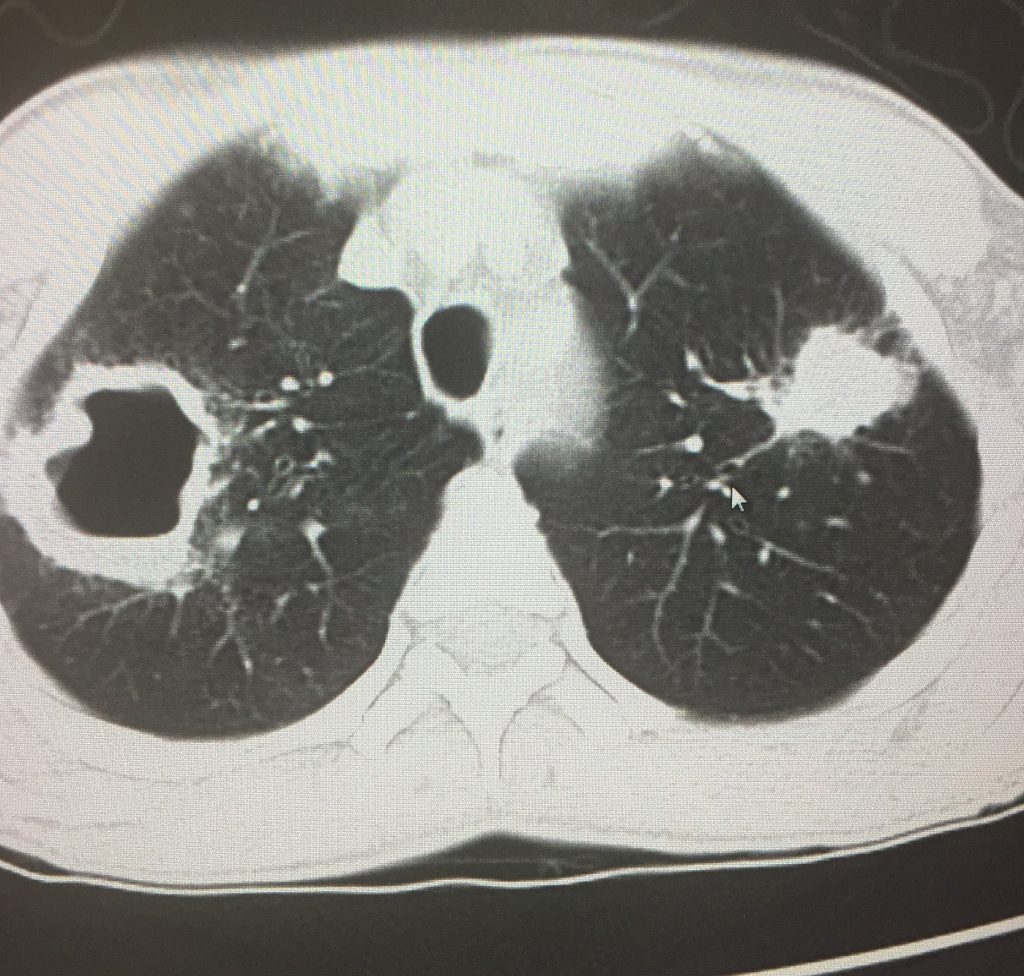
The differential diagnosis for a cavitary lesion in the lung as such boils down to three things:
Abscess
Tuberculosis
Lung Cancer
Here’s the crummy part: the ED physician doesn’t yet have all the data. We don’t have the benefit of a pulmonary consultation, ID consultation, culture results, anatomic pathology findings, etc. Yet we’re also about to [likely] never see the patient again as they are admitted to the floor. So how much do you tell them? Do you drop the ‘C’ word and destroy any chance of restful thoughts for the next 48 hours? Or do you commit a ‘lie of omission’ and leave that information out? After all, might it not be better to confirm that diagnosis before mentioning it? Would you want to know?
I chose not to mention cancer as a possibility, mostly because I placed myself in her shoes and I would probably not want that cloud hanging over me until it was confirmed.
In the case of our patient, labs were sent off and revealed a leukocytosis with left shift. She recalled having an impacted tooth a few months earlier that required surgery, after which she developed an abscess. The abscess was drained, she received IV antibiotics, and she thought it was all clear. On this visit she had a prolonged hospitalization wherein her cultures grew S. aureus. AFB smears were negative and she was ultimately discharged with a diagnosis of ‘bilateral lung abscess’ and ‘cavitary pneumonia’.