We’ve all experienced this: your overnight shift is winding down, you’re trying to wrap up dispositions on all of your patients, and you’re tired. You either discharge some people a little prematurely (those fluids will finish, they’ll feel better, and they’ll be able to leave. I’ll just finish the paperwork now and put in the discharge rack) or you give an abbreviated sign-out (chest pain, second enzyme pending, discharge home when negative).
Patient handoffs are high-risk encounters, especially in the ED. There’s a huge potential for breakdown in communication. In fact, poor communication is the leading cause of sentinel events within hospitals. Malpractice literature is saturated with communication breakdowns and one report claims this occurred in nearly 80% of medical malpractice lawsuits.
An elderly woman presented with left hip pain after a ground level fall. The overnight doctor ordered an x-ray and pain medication. He interpreted the x-ray as normal, wrote for some narcotics to go home with, and completed the discharge paperwork. Two hours later, at shift change, the oncoming nurse received report that the patient was waiting on her ride to come pick her up. She asked why we couldn’t send the patient to the waiting room to free up an ED bed, and was told ‘Oh, she won’t get up.’
Huh?
‘Oh, I know she can move her legs, because she uses them to get on/off a bedpan. But as soon as one of us goes in the room she acts like she can’t move it.’
Huh.
When I went in to re-evaluate this patient that we had not received any report on, she was noted to be in exquisite pain any time she moved the left hip. I ordered a CT scan and some labs, thinking we should prep for the potential for admission.
Here’s the CT:
Reviewing this led me to re-examine the initial x-ray:
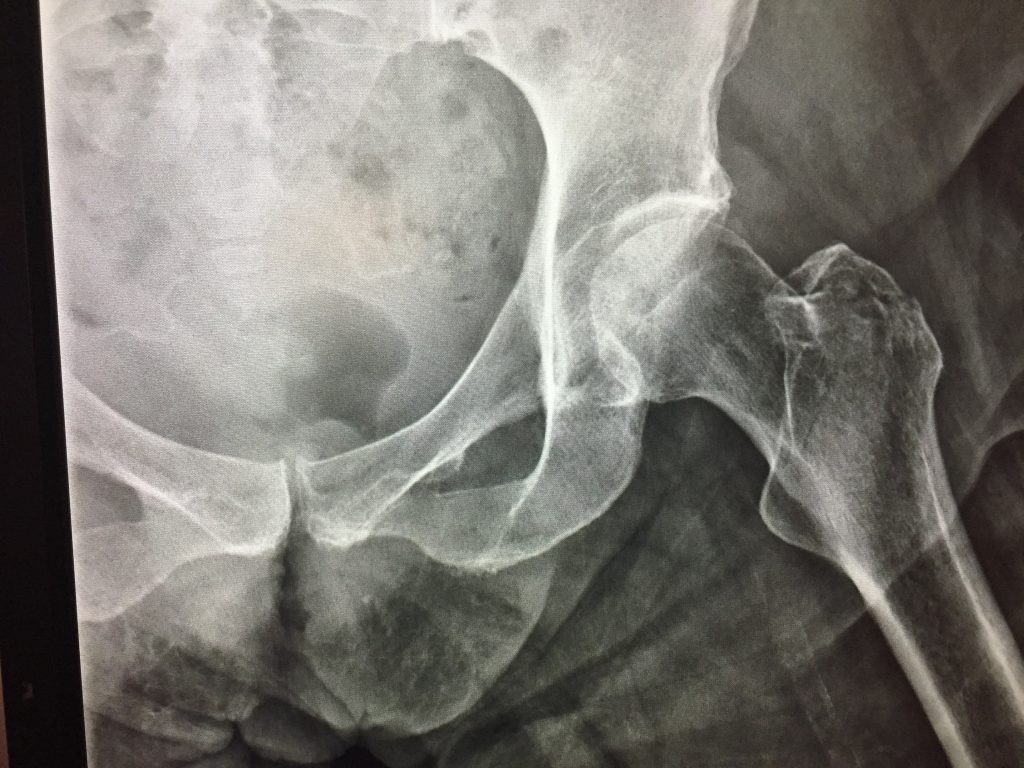

The official diagnosis is a left inter-trochanteric hip fracture. Hindsight is 20/20, Monday Morning quarterbacking isn’t fair – say whatever you want, but that fracture can be seen on the initial films. We all make mistakes and this can and has probably happened to me before: but if a patient remains in pain and your diagnostic tests aren’t being very…diagnostic – it may be time to further your workup. Patients with persistent post-traumatic hip pain with negative plain films deserve a CT scan. Period.
Be wary of patients that don’t want to leave. It’s easy to dismiss them but do so at your own peril. Hat-tip to an awesome nurse practitioner that remained steadfast in working this patient up.




