I’ll present this case in the actual sequence of events as they happened:
A patient in her mid-50s presented to the ED with chest pain. She saw her PCP and had an ECG done, after which he suggested that she go to an ED for some blood work and further evaluation. You don’t have that ECG available to start with, but one is run while the patient is here and brought to you to sign:
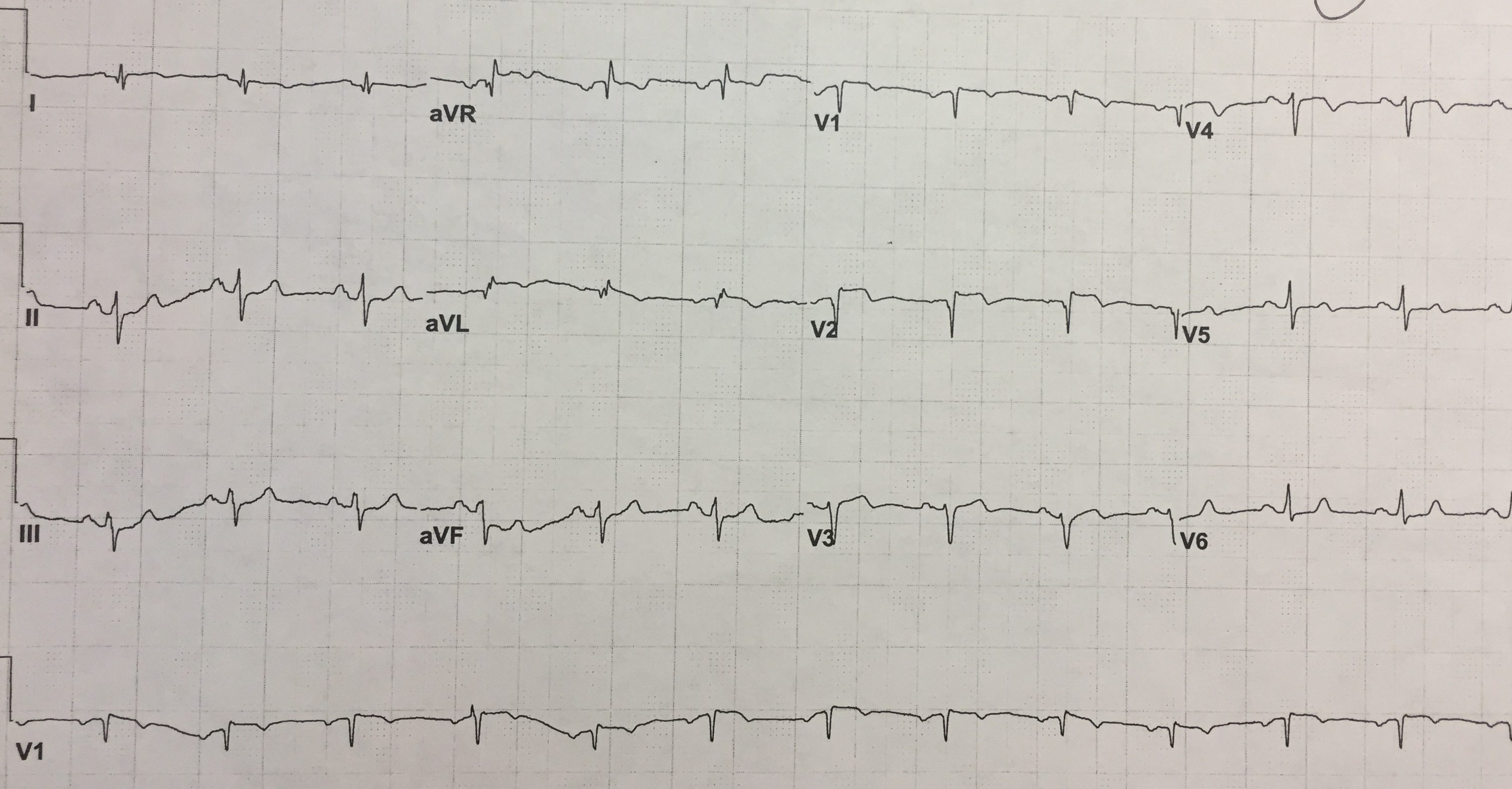
Without the benefit of seeing the patient, having vital signs, or even knowing why she is here, what conclusions can you make from this ECG?
There is ST elevation in leads V1-4 with reciprocal depression in the inferior leads.
This is the type of ECG that should, at the very least, get you to jump out of your seat and physically go the patient’s bedside. What I saw was a very calm and non-distressed patient who reported a 2 day history of chest pain but no pain currently. The ECG from her doctor’s office earlier today was at the bedside. Here’s how it looked:
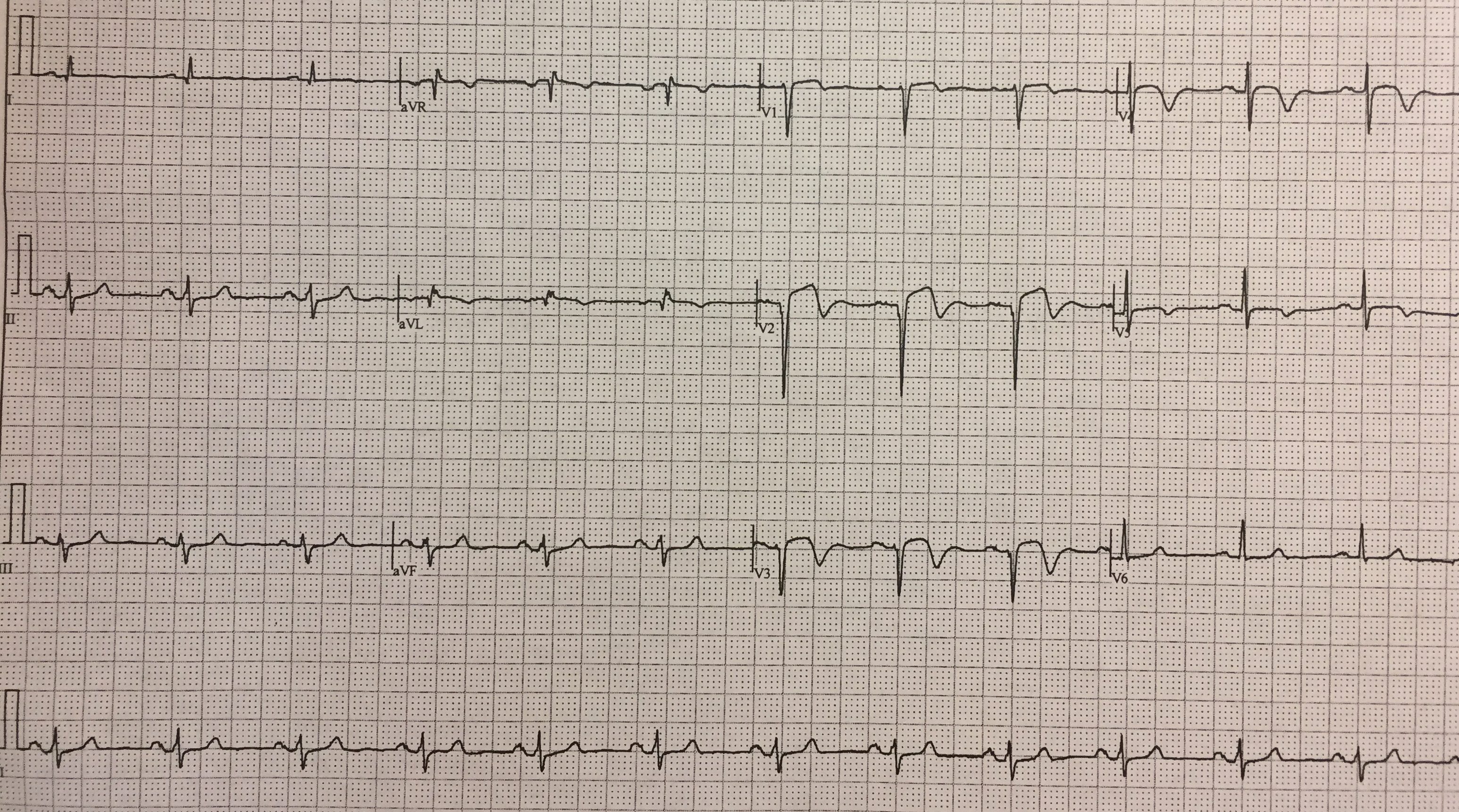

The ECG from the doctor’s office (technically the first ECG) shows biphasic T waves in V2-4. That should immediately bring to mind the eponym ‘Wellens Syndrome’.
Wellens’ syndrome is named after Dr. Hein J.J. Wellens, who first described the findings in 1982. Presence of the syndrome suggests critical proximal LAD stenosis.
This patient in fact had a 90% LAD lesion
Diagnostic criteria for Wellens Syndrome:
Little or no troponin elevation
Little or no ST elevation
Progressive symmetrical deep T wave inversion in leads V2 and V3
No precordial Q waves or loss of precordial R waves
Recent history of chest pain but pain-free at the time of ECG findings
Take-home points
-
-
- Wellens Syndrome represents a high-grade proximal LAD lesion until proven otherwise.
-
- There are other things that can present similarly, so don’t just hang your hat on Wellens.
-
- Performing a stress test in someone with this constellation of findings can be fatal – which is why it’s important to identify the condition. The workup starts with heart catheterization.
-




